概要
Amniocentesis is a procedure in which some of the amniotic fluid is removed for screening, diagnostic, and/or therapeutic purposes. The amniotic fluid is a thick consistency fluid that is present around the foetus in the womb. It helps in various functions like protection of foetus, maturation of organs, etc.
Various types of foetal cells and proteins are present in the amniotic fluid which can be used for analysis. Amniocentesis is useful for providing valuable information; however, you should understand the risks of this procedure and be prepared for the results too.
適応症
Amniocentesis is performed for different reasons. Some of the indications are:
- Genetic testing – amniocentesis provides information about foetal genetic make-up which can help diagnose certain conditions like Down syndrome.
- Pre-term delivery – amniocentesis is very useful in determining the health of a baby, especially degerming the health of your baby’s lungs. In some cases, e.g., if the mother has some complications, your baby might have to be delivered earlier than usual.
- Suspicion of foetal infection
- Polyhydramnios – this is a condition in which your womb has too much amniotic fluid which can be dangerous for your baby. Using amniocentesis, some fluid can be drawn out.
- You had positive results from a prenatal scan – if the result of a prenatal scan, i.e., first-trimester screen, are worrisome; you might be prescribed to get amniocentesis done.
- Age over 35 years – babies born to women 35 years or above have a higher risk of congenital complications. An example is down syndrome – the risk of your baby having down syndrome goes higher as you age.
- You have a family history of some genetic disease – this can include diseases like cystic fibrosis, sickle cell disease, thalassemia, phenylketonuria (PKU), etc.
- Abnormal ultrasound findings – your doctor might recommend an amniocentesis to diagnose or rule out certain conditions if they had a suspect during an ultrasound.
手順のリスク
Since the baby is very delicate, amniocentesis carries various risks which include:
- Leaking of amniotic fluid – although it is rare, amniotic fluid leaks through the vagina after amniocentesis. In most cases, however, the amount is very small and leakage stops after some days and the pregnancy continues normally.
- Needle injury – during the procedure, the baby might move their body, arm, or 足 which can come in front of the needle. The needle can injure the baby. However, these injuries are very rare.
- Uterine infection – very rarely, amniocentesis may trigger an infection in your uterus.
- Rh sensitisation – in a very small number of cases, it is reported that amniocentesis may cause the baby’s blood to come in contact with the mother’s blood. In case you have an Rh-negative blood group and your baby has an Rh-positive blood group, the baby’s blood is at risk of being attacked by your blood. This condition is preventable by the use of certain antibodies.
- Infection transmission – in case you have some infection; like hepatitis C, CMV, toxoplasmosis, or HIV/AIDS, the infection might get transferred to your baby during amniocentesis.
- Miscarriage – second trimester amniocentesis carries a small risk (0.1 – 0.3 percent) of miscarriage. Studies suggest that amniocentesis done before 15 weeks of pregnancy poses a greater risk of miscarriage.
You should keep in mind that amniocentesis is usually recommended when this test might have a significant impact on your baby or your health. Your doctor can only recommend it to you and you will have to decide to get an amniocentesis.
患者の準備
If your pregnancy is below 20 weeks at the time of amniocentesis, you should keep your bladder full, as this will support the uterus. In case, your pregnancy is 20 weeks or above you should empty your bladder before the procedure. Emptying your bladder will minimise the change of bladder puncture.
You will have to sign a consent form after the doctor explains the whole procedure to you. You should take someone from your family or some friend with you for emotional support.
手順
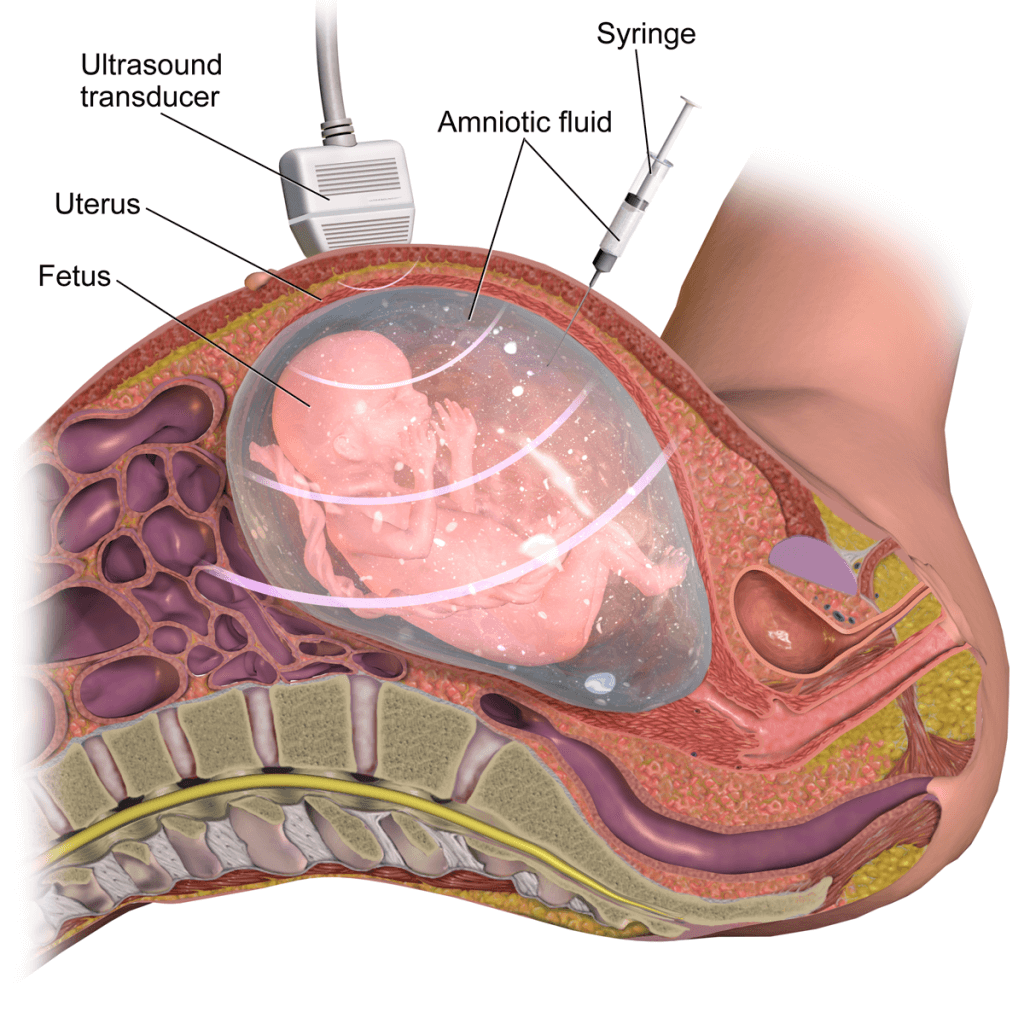
You’ll lie on your back on a flat table with your abdomen exposed. Your doctor will then perform an ultrasound to determine the baby’s exact location and position in the uterus. This will be visible on a monitor.
Next, your doctor will clean your abdomen with some antiseptic. Most of the women are not given any anaesthetics. Most women complain of mild discomfort only during amniocentesis.
Then, your doctor will insert a thin hollow needle that is attached to a syringe. This needle is guided by ultrasound. A small amount of amniotic fluid is then drawn out of the amniotic sac. The amount of fluid that needs to be taken depends on the age of your pregnancy.
You might feel slight cramping or stinging when the needle enters your uterus or while the fluid is being taken out, however, you should stay still.
患者の回復
After the procedure, you might feel some cramping or slight discomfort. Your doctor will continue using the ultrasound to monitor your baby’s heart and health.
You should consider avoiding strenuous exercise for about a few days; however, you can resume your other normal activities after the procedure.
次のような症状が見られた場合は、医師にご相談ください。
- Vaginal bleeding or loss of amniotic fluid through the vagina
- Severe uterine contraction or cramping lasting for an hour or more
- 高熱
- Redness, or swelling around the site of needle insertion
- Unusual foetal activity or lack of foetal movement
結果
The amniotic fluid sample will be sent to the lab for testing. Your doctor or genetic consultant will help you understand your results once they come in. it usually takes about a week or two to get the results. In emergency conditions, the results can be expedited.
Amniocentesis can be used to identify genetic conditions, but not all of the congenital conditions can be diagnosed by this test. You might be able to make big decisions like whether to continue your pregnancy or not. You should get proper counselling and take someone with you for emotional support.
Amniocentesis can give an accurate indication of whether the foetal lungs are mature enough to survive after birth or not. This information can reassure you that your baby is safe for birth.
- Ghidini A, et al. Diagnostic amniocentesis. https://www.uptodate.com/contents/search. Accessed Oct. 11, 2018.
- Cunningham FG, et al., eds. Prenatal diagnosis. In: Williams Obstetrics. 25th ed. New York, N.Y.: McGraw-Hill Education; 2018. https://accessmedicine.mhmedical.com. Accessed Oct. 11, 2018.
- Amniocentesis. American Pregnancy Association. http://americanpregnancy.org/prenatal-testing/amniocentesis/. Accessed Oct. 11, 2018.
- Papadakis MA, et al., eds. Genetic & genomic disorders. In: Current Medical Diagnosis & Treatment 2018. 57th ed. New York, N.Y.: McGraw-Hill Education; 2018. https://accessmedicine.mhmedical.com. Accessed Oct. 11, 2018.
- American College of Obstetricians and Gynecologists (ACOG) Committee on Practice Bulletins – Obstetrics. ACOG Practice Bulletin No. 162: Prenatal Diagnostic Testing for Genetic Disorders. Obstetrics & Gynecology. 2016;162:1. https://www.acog.org/-/media/Practice-Bulletins/Committee-on-Practice-Bulletins—-Obstetrics/pb162.pdf?dmc=1&ts=20181012T2016340336. Accessed Oct. 12, 2018.
Health Literacy Hub Webサイトで共有されるコンテンツは、情報提供のみを目的として提供されており、州または国の資格のある医療専門家が提供するアドバイス、診断、または治療に代わるものではありません。読者は、他の情報源から提供された情報を確認し、自分の健康に関して質問がある場合は、資格のある開業医のアドバイスを求めることをお勧めします。 Health Literacy Hubは、提供された資料の適用から生じる直接的または間接的な結果に対して責任を負いません。