Overview
Colorectal cancer (CRC), also known as bowel cancer, is the fourth leading cause of death worldwide. It develops from the large intestine and usually begins with small and dense cellular masses of healthy tissue, called polyps or adenomas, which adhere to the internal walls of the colon or rectum. Over time, these polyps may grow and convert into cancerous tissue, with a variable prognosis depending on the extent and spreading of the tumour.
The different stages of cancer progression (staging) go from 0 (early stage) to IV (advanced stage) and are defined based on the size of the tumour, the spread to the near lymph nodes, and the level of metastasis, or diffusion to distant lymph nodes or organs.
Early detection is associated with improved patient outcomes through the surgical excision of premalignant lesions (polypectomy) that may undergo cellular transformation. Therefore, screening programs have been rolled out in many countries aiming to reduce the burden of CRC, which is projected to reach over 1.5 billion people by 2050.
Signs and Symptoms
Routine screening programs for CRC targeting individuals between 50- and 75-years old aim to achieve timely detection of early signs of the disease and subsequent intervention. Nevertheless, 80% of the CRCs are detected when patients present to the medical practitioner with suspicious signs and symptoms, which include rectal bleeding, abdominal pain, and anaemia. Rare but serious consequences of CRC include obstruction of the large bowel, peritonitis, and perforation, which are all treated as a medical emergency and may be associated with metastatisation of cancer.
Causes and Risk Factors
As per many other cancer types, the causes underlying the formation and transformation of colorectal polyps is not fully understood. Nevertheless, various environmental factors influencing the incidence rate for sporadic CRC (over 50 years old) have been identified, and these include the increase in the aging population and unhealthy dietary habits (high-sugar diet, smoking, obesity, lack of physical activity).
Inherited forms of CRC account for 35% of all cases, and these can be classified into hereditary CRC or Familial CRC.
Hereditary CRC is generally characterised by an autosomal dominant pattern associated with increased risk below 50 years of age. The two most common manifestations of this form are the Familial Adenomatous Polyposis, or FAP, caused by a pathogenic genetic mutation in the APC gene, and the Lynch syndrome, also known as Hereditary Non-Polyposis Colorectal Cancer (HNPCC), caused by defects in the DNA mismatch repair mechanism or epigenetic regulation.
Non-syndromic or familial CRC is distinguished by the hereditary form of CRC because it encompasses both patients with unidentified inherited traits and others with a sporadic form that aggregates in the family, suggesting a role for genetic susceptibility amongst younger patients.
Diagnosis
Clinical evidence has shown that CRCs frequently arise from adenomatous polyps that typically acquire dysplastic changes in a 10 to 15-year period before developing invasive carcinoma, and the early detection-removal of polyps will reduce the incidence of CRC.
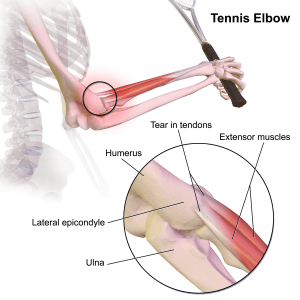
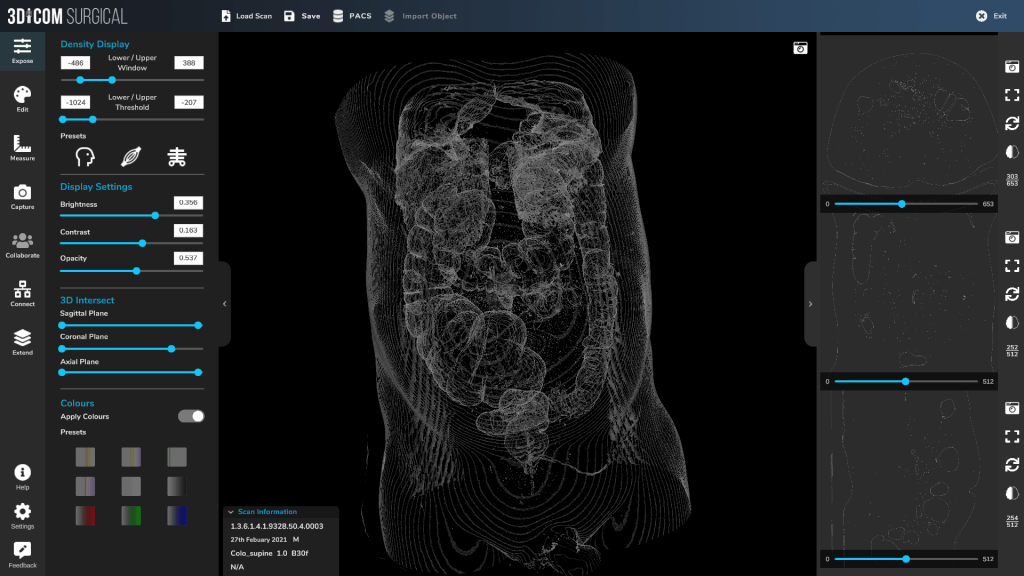
The gold standard diagnostic exam for the screening of colorectal cancer is called an optical colonoscopy, which involves the insertion of a long flexible tube, equipped with a micro camera, that is inserted in the patient’s rectum to record and detect the presence of polyps within the colon. The exam is invasive, uncomfortable for patients, and requires long preparation and pharmacological sedation with a consequent impact on the patient’s recovery following the procedure. Moreover, colonoscopy is associated with a risk of tearing and bleeding from the colon or rectum wall, and cramping and bloating may also occur. Due to the invasive nature of this procedure, over the years a less invasive procedure, known as Virtual Colonoscopy, have been developed. This approach relies on the ability of Computed Tomography (CT) scans to generate cross-sectional images of the abdomen following inflation of the rectum. The procedure is minimally invasive, and it can be performed in just a few minutes, with limited discomfort and recovery time for patients. Nevertheless, technical limitations related to the adoption of CT scans and the inability to detect polyps smaller than 5 mm in diameter has represented a limitation to the primary application of this procedure.
Treatment
Treatment for CRC is largely relying on endoscopic mucosal resection of adenomatous polyps which is performed during a colonoscopy. The procedure also enables the collection of samples for histopathological analysis to determine whether cancer has invaded the submucosa layers. Although this endoscopic procedure is less invasive than a standard surgery and is associated with a faster and better recovery, potential complications include the risk of bleeding, infection, and perforation to surrounding organs.
If metastatic disease is confirmed, surgical resection may be required, and depending on the medical case, radiotherapy and neoadjuvant chemotherapies may be recommended to augment the chances of treatment success. In the presence of non-surgical colon cancer cases, palliative cures finalised to improve the patient’s quality of life and prolong life expectancy may be recommended by the medical specialist.
The content shared on the Health Literacy Hub website is provided for informational purposes only and it is not intended to replace advice, diagnosis, or treatment offered by qualified medical professionals in your State or Country. Readers are encouraged to confirm the information provided with other sources and to seek the advice of a qualified medical practitioner with any question they may have regarding their health. The Health Literacy Hub is not liable for any direct or indirect consequence arising from the application of the material provided.