Overview
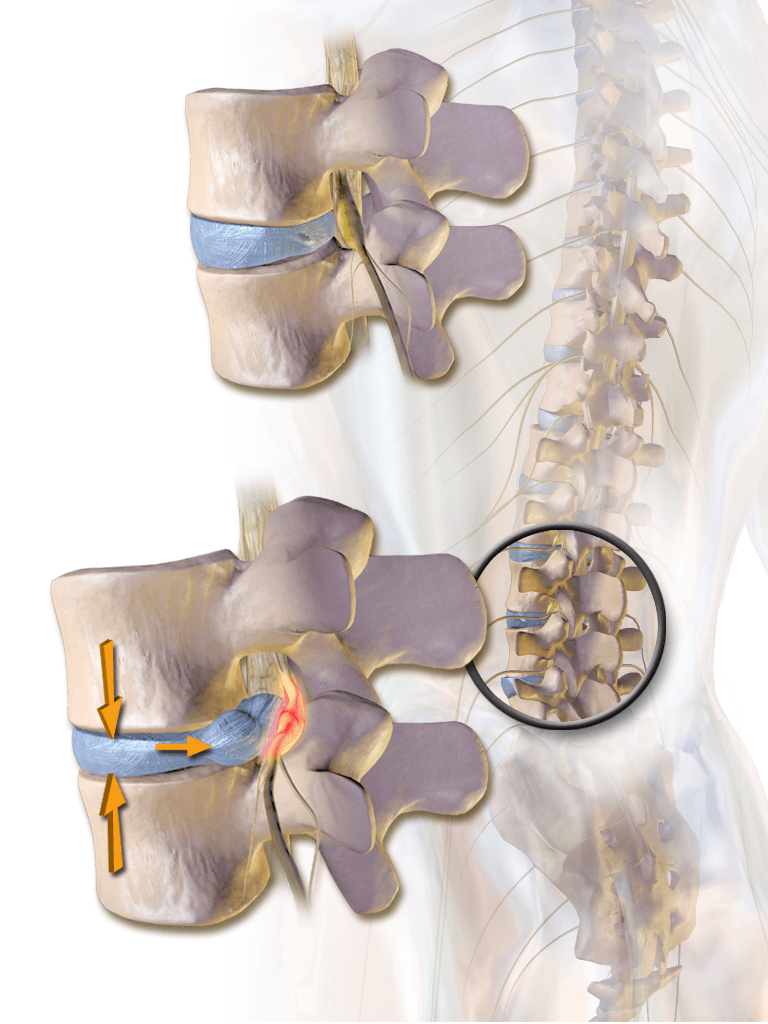
A disc refers to the cushiony fluid present between your vertebrae. The vertebrae are bones that stack up to make your spine and they are separated by discs in between. A disc is made up of a central soft jelly-like substance called the nucleus pulposus and an outer surrounding fibrous substance called annulus fibrosus.
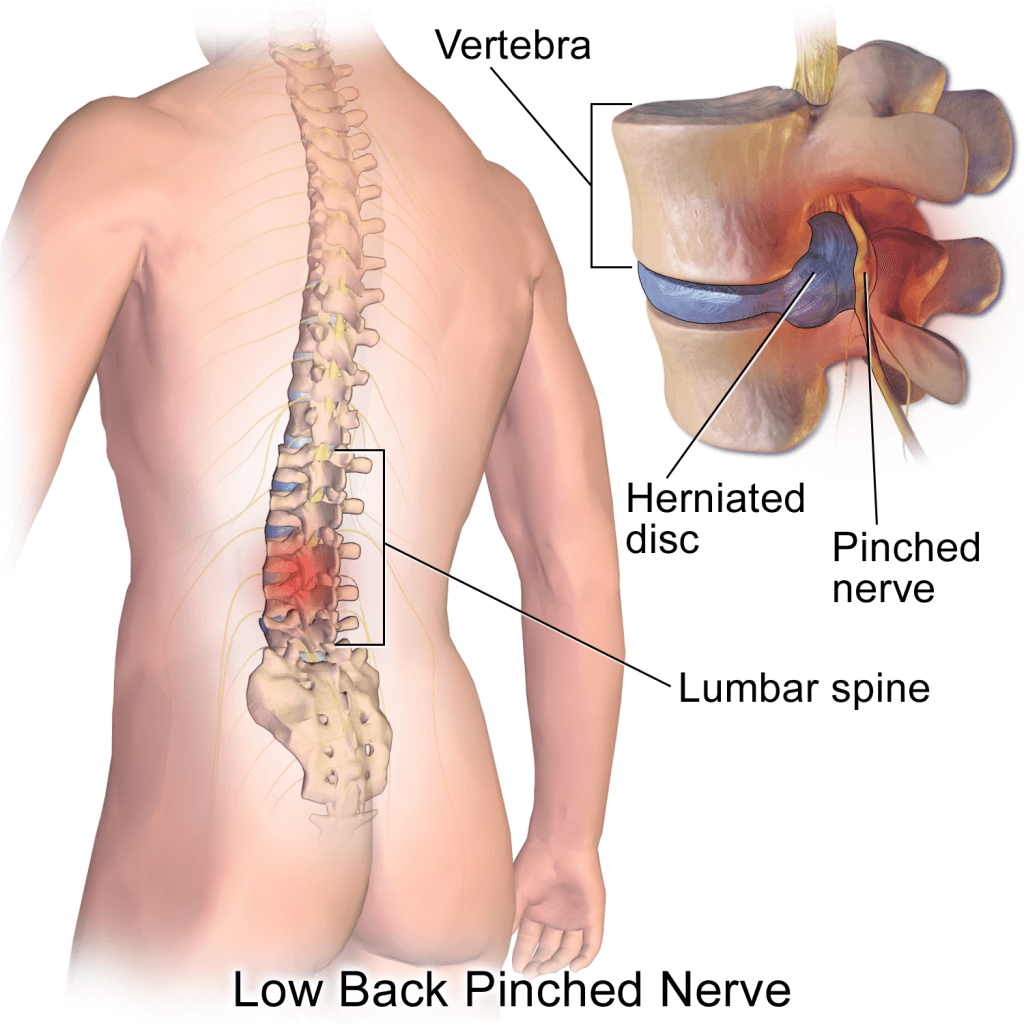
A disc herniation is also known as a slipped disc or a ruptured disc refers to a condition in which the inner substance (nucleus) of your disc is pushed out through a weakened or ruptured annulus (outer covering of disc). A herniated disc can occur anywhere in the spine however it is more common at some vertebral levels than others. It is oftentimes a very painful condition as the protruding disc can compress the nearby spinal nerves.
It is a fairly common problem affecting 5 to 20 per 1000 adults annually. In this article, we will look at some of the symptoms, causes, and treatments available for a herniated disc.
Signs and Symptoms
The most commonly herniated disc occurs at the level of lumbar or cervical vertebrae, which refer to the lower back and neck region, respectively. The signs and symptoms of a disc herniation depend upon the site of the herniation and the extent to which the nucleus (inner substance) is compressing the nearby spinal nerves.
Symptoms usually start unilaterally i.e., on one side and the symptoms include:
- Arm or leg pain – a disc herniation in the lower back will cause symptoms in the lower back or legs, while a disc herniation in the neck regions will present symptoms in the neck and arm region.
In the case of the former, you might feel:
- Pain in the lower back that is radiating downwards in your buttocks, thighs (back or side), or down your foot. This type of pain is also called sciatica.
- Numbness in your lower back and your thighs.
- Tingling or burning feeling in your lower back, buttocks and thighs.
- Weakness in moving your legs
- Difficulty in standing from sitting position.
In case of a cervical disc herniation, you may experience:
- Pain in your neck radiating down towards your shoulder and arm
- Neck stiffness
- Headache
- Numbness and tingling in your arm or fingers
- Weakness in moving your arm and gripping things
In some cases, you might have a herniated disc without having any signs or symptoms. In this case, the herniated disc is not compressing any surrounding tissue and your injury is very minor.
If you experience, extreme radiating pain with loss of bladder or bowel control you should immediately see your doctor and seek help.
Causes and Risk Factors
Disc herniation is mostly caused by a gradual weakening of the protective annulus fibrosus due to wear and tear. Conversely, it can be caused by excessive sustained pressure on the nucleus pulposus which drives it out of its compartment through the annulus. As you age your annulus becomes stiffer and more prone to rupture due to pressure from the nucleus.
In some cases, disc herniation is caused by excessive weight lifting, twisting, or turning with a bad posture, and, less commonly, by a traumatic accident (fall on the back or hips).
Risk factors leading to disc herniation include:
- Weight – increased weight puts more pressure on the disc making it easier for the annulus to tear
- Occupation – jobs that require heavy object lifting from the floor can over time put a strain on your discs making them weak. On the other hand, sitting for long hours, especially in flexed (curved forward) posture puts a lot of bad pressure on your discs leading to disc herniation
- Looking down for too long – can put a strain on the vertebrae in your neck
- Genetics – some people inherit a predisposition to a disc herniation from their family
- Smoking – it is proposed that smoking decreases the oxygen delivery to the tissues in your disc holding it together. Decreased oxygen can cause tissue damage and weakening of the annulus
Diagnosis
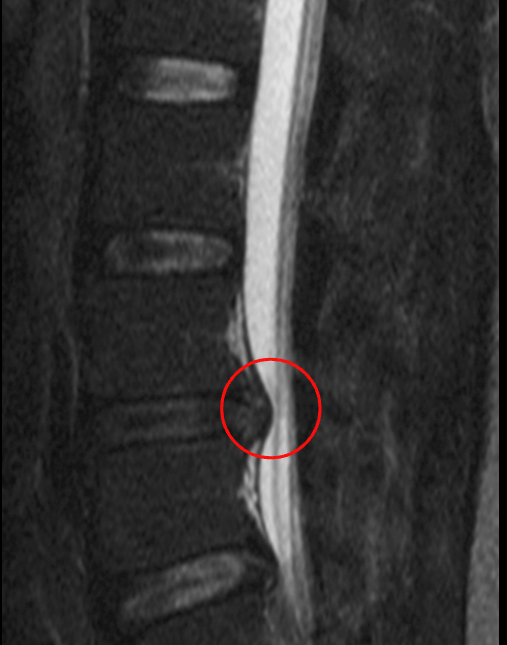
Your doctor will make a diagnosis based on your medical history and physical examination. A CT scan (advance type of X-ray) and MRIs are usually used to confirm a diagnosis of disc herniation and to point out the exact location of the herniated disc. Other imaging techniques include X-ray and myelogram. A myelogram is a technique in which a dye is injected into your spinal fluid and then an X-ray is taken.
Physical examination may include neurological examination:
- Checking for reflexes
- Muscle strength
- Walking gait i.e., if you are walking properly
- Moving your neck, arm, or leg in a different position and assessing your pain or discomfort
Usually, a history and physical examination are enough to make a diagnosis of disc herniation.
Treatment
Most patients usually need conservative and symptomatic treatment. These treatment options include:
- Resting – lying down on a firm plane mattress (not hard) is recommended. You should rest as much as you can until your symptoms reduce or go away
- Avoid picking up stuff or bending forward
- Sitting with your back resting against a support
- Avoid movement for a long time i.e., standing, walking, or climbing up the stairs
- Medications – over the counter NSAIDs are most commonly used to alleviate pain associated with disc herniation. Other medication may include medicine that reduces radiculopathy (traumatic damage to the nerves).
Muscle relaxants, steroids, and opioids are also used in chronic (long-term) patients to reduce pain and inflammation
- Physical therapy – physical therapy like heat pads, massages, the muscular stimulator can help regain strength and reduce symptoms at a faster rate
- Nutritional supplements – vitamin D, B12, and calcium are often prescribed along with conservative treatment to strengthen the bones and muscles in general
In severe cases of disc herniation i.e., in which you might lose bladder or bowel control, surgery is required to repair the annular ligament and push the herniated disc back.
Complications and Prevention
Complications
Severe compression of nerves can cause some severe complications including:
- Paraplegia and inability to walk – paralysis of legs
- Loss of bowel and bladder control – the nerves supplying your intestines and bladder originate below your waist. Injury at this level can cause loss of your urine and defecation control
Prevention
To help yourself preventing disc herniation you should:
- Exercise regularly – exercise can strengthen your muscles and ligaments which can keep your disc intact, especially swimming and jogging
- Reduce your weight
- Using a protective weightlifting belt during lifting heavy weight
- Eat whole food in a balanced diet
- Maintain a good posture
- Avoid sitting for a very long time
- Quit smoking
- Herniated disc. American Association of Neurological Surgeons. https://www.aans.org/en/Patients/Neurosurgical-Conditions-and-Treatments/Herniated-Disc. Accessed Aug. 20, 2019.
- AskMayoExpert. Herniated disc. Mayo Foundation for Medical Education and Research; 2019.
- Levin K, et al. Acute lumbosacral radiculopathy: Treatment and prognosis. https://www.uptodate.com/contents/search. Accessed Aug. 20, 2019.
- Herniated disk. American Academy of Orthopaedic Surgeons. https://orthoinfo.aaos.org/en/diseases–conditions/herniated-disk/. Accessed Aug. 20, 2019.
- FAQs before EDX testing. American Association of Neuromuscular & Electrodiagnostic Medicine. https://www.aanem.org/Patients/FAQs-before-EDX-Testing. Accessed Aug. 20, 2019.
- Herniated disk in the lower back. American Academy of Orthopaedic Surgeons. https://orthoinfo.aaos.org/en/diseases–conditions/herniated-disk-in-the-lower-back/. Accessed Aug. 20, 2019.
- Shelerud RA (expert opintion). Mayo Clinic. Aug. 26, 2019.
- https://www.ncbi.nlm.nih.gov/books/NBK441822/
The content shared in the Health Literacy Hub website is provided for informational purposes only and it is not intended to replace advice, diagnosis, or treatment offered by qualified medical professionals in your State or Country. Readers are encouraged to confirm the information provided with other sources, and to seek the advice of a qualified medical practitioner with any question they may have regarding their health. The Health Literacy Hub is not liable for any direct or indirect consequence arising from the application of the material provided.