Overview
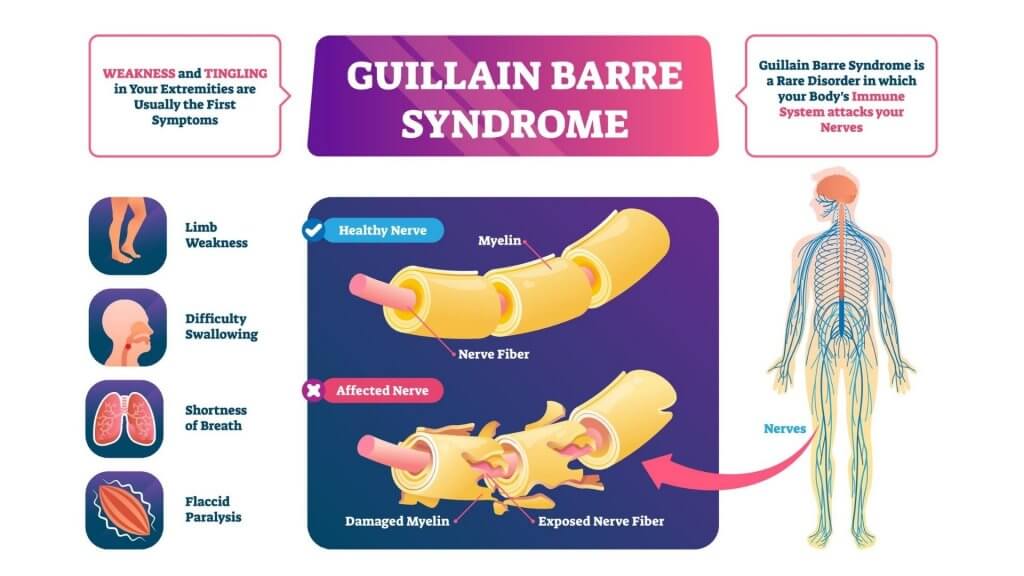
Guillain-Barre (gee-YAH-buh-RAY) syndrome is a rare and serious autoimmune pathology (a disorder of the body), in which your nerves are attacked by your immune system. It is characterized by numbness, weakness, and pain in your body parts especially your hands, feet, and limbs. It often presents as an ascending paralysis i.e.; your feet start paralysing first followed by your legs and upper body respectively.
Severe forms of Guillain-Barre syndrome require emergency treatment and hospitalization. According to some researches, GBS occurs with a median annual incidence of 1.3 cases per 100,000 people across the world. In Australia, there are around 340 cases reported per year.
In this article, we will highlight the symptoms, causes, treatment, and prevention of Guillain-Barre syndrome.
Signs and Symptoms
As mentioned above, GBS often starts as numbness and tingling in your extremities starting especially from the feet and spreading to your arms and upper body. In few cases, however, this neuropathy (a problem associated with your nerves) appears first in the arms and face. Some common manifestations of GBS include:
- Pin prickling or needles sensations in your feet or hands
- Weakness and pain in your legs spreading upwards towards your trunk
- Instability while walking or climbing stairs
- Severe muscular or joint pain in your limbs
- Difficulty in seeing or focusing properly from your eyes
More severe symptoms include:
- Difficulty or loss of bladder control and bowel control
- Tachycardia. Rapid heart rate over 100 bpm
- Hypertension (high blood pressure) or hypotension (low blood pressure)
- Difficulty in swallowing, chewing, and facial paralysis
- Difficulty breathing
In most cases, the severity of GBS peaks almost 2 weeks after the symptoms appear, and professional medical aid is required.
Types
Guillain-Barre syndrome occurs in several forms. The main types include:
- Acute Inflammatory demyelinating polyradiculoneuropathy (AIDP) – this is the most common presenting form. This condition presents, usually, as musculoskeletal weakness in your lower body which spreads towards your upper body
- Miller Fisher syndrome (MFS) – MFS is more common in Asia. It begins as paralysis in the eyes. Other clinical presentations include unsteady gait (walking pattern) and instability
- Acute motor axonal neuropathy (AMAN) and acute motor-sensory axonal neuropathy (AMSAN) – these forms are more prevalent in China, Japan, and Mexico. It can involve sensory loss e.g., diminished feeling on the skin
Causes and Risk Factors
The exact cause of Guillain-Barre is still unknown; however, it is thought to be associated with a problem in the immune system, your body’s natural defense system against illnesses. It usually appears some days or weeks following a digestive or respiratory tract infection. Your immune system starts attacking your nerves instead of other pathogens, which can cause inflammation and death of the peripheral nerves (nerves outside the brain and spinal cord). In AIDP, the myeline sheath is damaged which affects the signal delivery in the nerves. Myeline sheath is the protective covering around your nerves that helps in the movement of signals across the nerves.
Certain diseases, infections, and age can determine the risk you carry for acquiring GBS. These risk factors include:
- Age – increasing age increases the risk of getting GBS
- Males are affected more than females with a male to female ratio of 1.5:1
- Most commonly it is associated with a bacterial infection from Campylobacter jejuni. Campylobacter is a bacterium that can be transmitted through undercooked poultry and is associated with GBS
- Influenza virus
- Cytomegalovirus (CMV)
- Epstein-Barr virus (EBV)
- Zika virus
- In rare cases, some vaccination e.g., influenza or other childhood vaccinations
An infection with the COVID-19 virus and COVID-19 vaccination (Johnson and Johnson) have also been seen to be the cause of Guillain-Barre syndrome.
Diagnosis
It is often hard to diagnose GBS in its early stages due to the similarity of the symptoms with other neurological disorders. Your physician will start taking your history and perform a physical examination. Your physician might recommend getting:
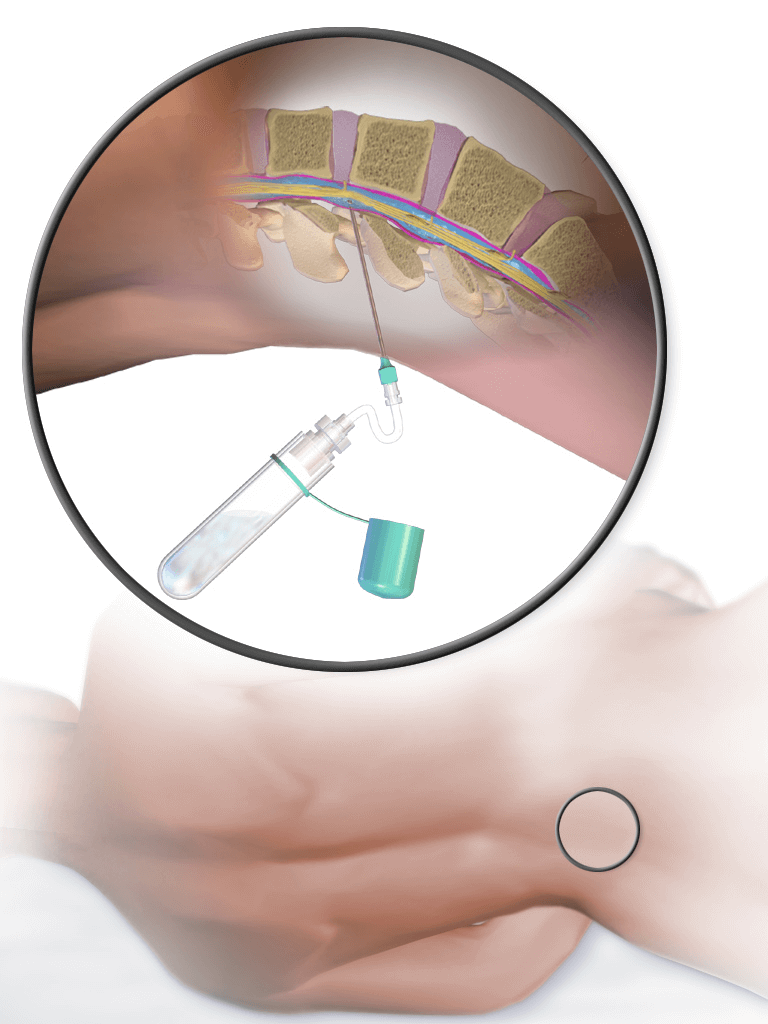
- Spinal tap or Lumbar puncture – a small sample of your CSF (cerebrospinal fluid), present in your brain and spinal cord, is withdrawn inserting a needle in your lower back. The fluid is then tested for changes that are specific to GBS and the GBS causing bacteria such as Campylobacter
- Electromyography – a technical procedure used to assess the muscular activity of different parts of your body. This is done with the help of thin-needle electrodes
- Nerve conduction studies – a similar technique to electromyography in which small electrodes are placed on your skin and electrical shocks are used to activate the nerves. This is then used to measure the response that the muscle produces to that shock
Treatment
GBS is an incurable disease i.e., there is not a curable treatment for GBS. However, there are a couple of symptomatic treatment options that can help you recover at a faster rate and reduce the severity of your disease:
- Intravenous Immunoglobulin (IVIG) therapy – immunoglobulins (IG) from healthy individuals are given through a vein. Immunoglobulins are small defense particles that your body produces to fight the disease-causing agents. High doses of IGs prevent the autoantibodies (antibodies against own cells) from damaging the nerves, which might be a cause of Guillain-Barre syndrome.
- Plasma exchange (plasmapheresis) – in this technique, the fluid portion of your blood (plasma) is separated from your blood cells and your blood cells are then put back. The blood cells then synthesise more new plasma. This fresh plasma can help get rid of certain antibodies that might be triggering the destruction of your peripheral nerves.
Oftentimes, these two therapies are done side by side or in an alternating fashion, and it has shown to produce better results. Other treatment options include:
- Medication – to relieve pain and prevent blood clots (occur due to immobility)
- Physical therapy – you might need physical therapy during and after your recovery to increase muscular coordination and quicken the recovery.
Complications
GBS is a nerve-affecting disease that can produce several complications especially in cases of inadequate treatment. You may experience:
- Breathing difficulties
- Residual numbness or weakness – numbness or weakness after your recovery
- Cardiovascular problems – blood pressure or heart problems can be a significant outcome of GBS
- Bladder and bowel function problems – urinary incontinence (unable to hold your urine ) etc.
- Blood clots – immobility due to GBS can cause blood flow in your veins to become sluggish causing blood clots
- Relapse – according to some data 2 – 5% of the people once affected with Guillain-Barre syndrome experience recurring the disease (relapse)
Prevention
Since the cause and exact pathophysiology (disease mechanism) behind Guillain-Barre syndrome is not understood properly, there are no set guidelines for preventing GBS. However, you can prevent the infections that cause GBS by:
- Properly cooking food at high temperatures
- Sanitising and keeping a good hygiene
- Wijdicks EFM, et al. Guillain-Barre syndrome. Mayo Clinic Proceedings. 2017;92:467.
- Willison HJ, et al. Guillain-Barre syndrome. The Lancet. 2016;388:717.
- Guillain-Barre syndrome fact sheet. National Institute of Neurological Disorders and Stroke. https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Guillain-Barr%C3%A9-Syndrome-Fact-Sheet. Accessed March 16, 2017.
- Vriesendorp FJ. Clinical features and diagnosis of Guillain-Barre syndrome in adults. http://www.uptodate.com/home. Accessed March 16, 2017.
- Vriesendorp FJ. Guillain-Barre syndrome: Pathogenesis. http://www.uptodate.com/home. Accessed March 16, 2017.
- Ferri FF. Guillain-Barre syndrome. In: Ferri’s Clinical Advisor 2017. Philadelphia, Pa.: Elsevier; 2017. https://www.clinicalkey.com. Accessed March 16, 2017.
- Vriesendorp FJ. Guillain-Barre syndrome in adults: Treatment and prognosis. http://www.uptodate.com/home. Accessed March 16, 2017.
- Ryan MM. Guillain-Barre syndrome in children: Treatment and prognosis. http://www.uptodate.com/home. Accessed March 16, 2017.
- Brown AY. Allscripts EPSi. Mayo Clinic. April 17, 2020.
- Leonhard SE, et al. Diagnosis and management of Guillain-Barre syndrome in ten steps. Nature Reviews Neurology. 2019; doi:10.1038/s41582-019-0250-9.
- McIntosh K. Coronavirus disease 2019 (COVID-19). https://www.uptodate.com/contents/search. Accessed Sept. 15, 2020.
- COVID-19: Vaccination. AskMayoExpert. Mayo Clinic; 2021.
The content shared in the Health Literacy Hub website is provided for informational purposes only and it is not intended to replace advice, diagnosis, or treatment offered by qualified medical professionals in your State or Country. Readers are encouraged to confirm the information provided with other sources, and to seek the advice of a qualified medical practitioner with any question they may have regarding their health. The Health Literacy Hub is not liable for any direct or indirect consequence arising from the application of the material provided.