Overview
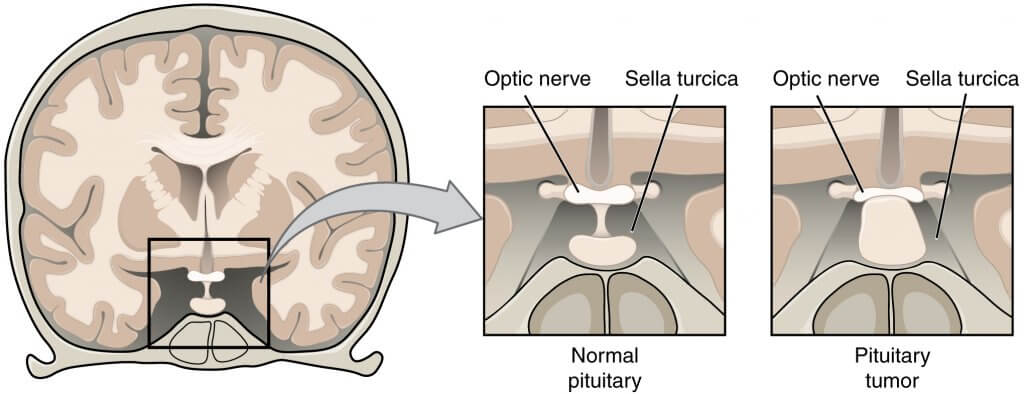
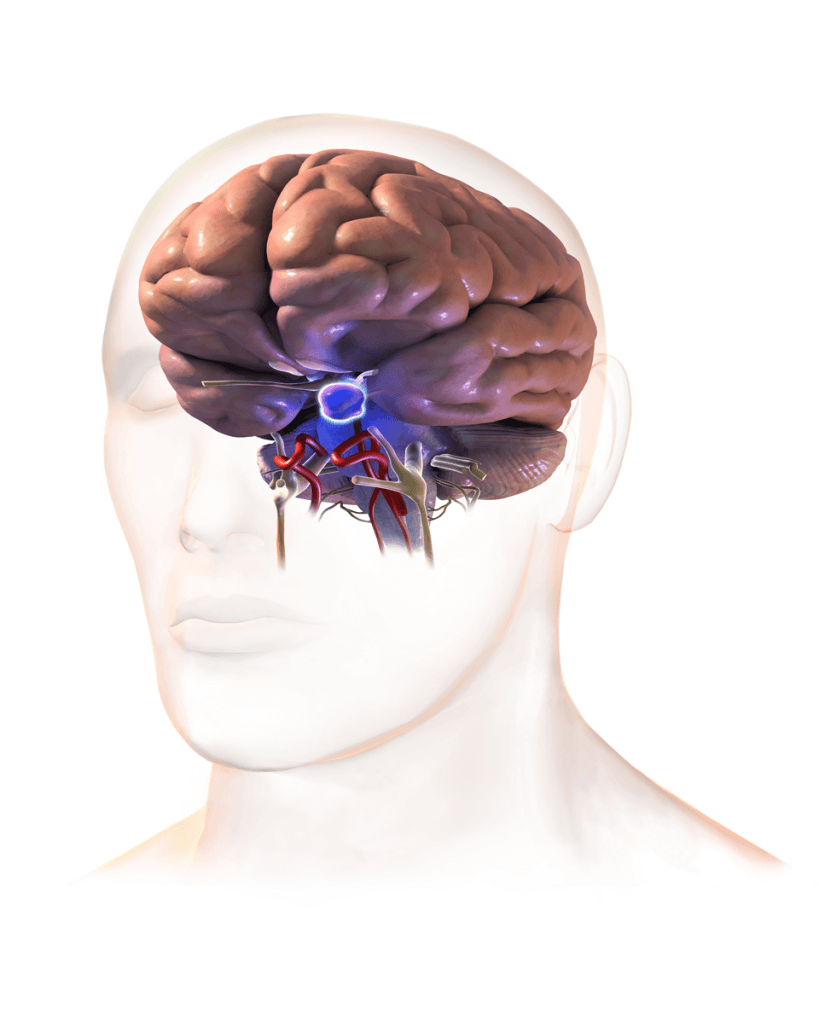
The pituitary gland is a pea-sized gland located in the cranial cavity (skull). Due to its vastly interconnected effects on almost all of the organs in the body, it is often referred to as the master gland of our bodies. A gland is an organ in the body that produces secretions that have various effects on the body.
A pituitary adenoma is an abnormal growth in the cells of the pituitary gland. It is considered a benign tumour of the pituitary gland. A benign tumour refers to an abnormal (cancerous) cell growth that does not have the potential to metastasize (travel) in other organs of the body e.g., blood, liver, etc. according to some analysis, pituitary adenomas consist of 15% of the total intracranial tumours.
Clinically significant (symptoms producing) pituitary adenomas are reported by almost 75- 95 out of 100,000. In Australia, the cases of Pituitary adenoma are rising with an average of 1 in 1000 people. In this article, we will discuss some facts regarding pituitary adenoma and how you can get the treatment.
Signs and Symptoms
Because of its relation to a gland, the pituitary adenoma interferes with the secretion of the pituitary gland. This can lead to various problems in your body. Hence, the symptoms vary depending upon the type of cells involved and the excess hormone being produced. Having excess hormones can lead you to have:
- Excess Growth hormone (GH) – this can result in gigantism in children and acromegaly in adults. Both of these conditions exhibit abnormal increase size of the body or some parts of the body
- Excess adrenocorticotropic hormone (ACTH) – this can cause excess steroid production in your body known as Cushing’s disease. Your feet and hands get puffy and you have swelling in various parts of your body
- Excess thyroid releasing hormone (TSH) – this can exacerbate your thyroid hormone production and lead you to hyperthyroidism, a relatively life-threatening disease
Some common symptoms associated with pituitary adenoma are:
- Headaches
- Vision problems – including double vision or blurry vision
- Loss or change in the sense of smell
- Nausea associated with vomiting
- Failing to hit puberty
- Unexplained weight loss or weight gain
- Excessive swelling of face, legs, or abdomen
- Sexual disfunction
- Menstrual problems in females – absent periods or excessive bleeding
Causes
As for a lot of other cases of abnormal cell growth (tumour formation), the cause of abnormal cell growth in the pituitary gland is unknown. Some medical professionals have attributed it to damage in the DNA. DNA is the component of your cell that controls your cell’s activities and its division (reproduction). Damages to the DNA can cause uncontrolled cellular reproduction which can eventually turn into a tumour.
Risk Factors
If you have a family history of some type of cancer especially multiple endocrine syndrome – type 1 (MEN 1), you have an increased risk of pituitary adenomas. In simple words, if someone in your first relatives have this disease you are at more risk of having it. MEN 1 is characterized by multiple tumorous growths in different glands of your body including the pituitary gland. You can get your genetic test done to check if you have this disease.
Trauma to the head can also increase your chances of getting a pituitary adenoma.
Diagnosis
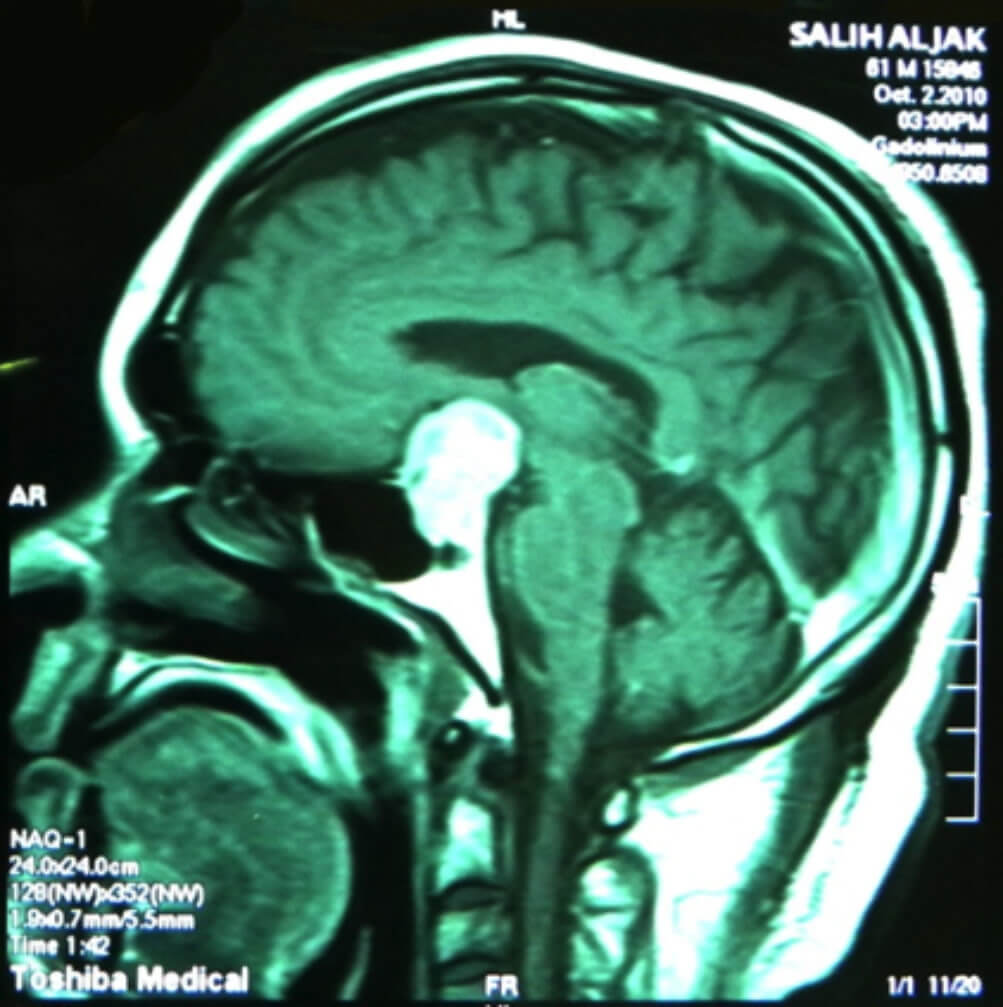
Your doctor will do a thorough review of your symptoms and your medical background plus your physical exam. If your doctor suspects that you have pituitary adenoma, he or she will require lab tests to be done along with multiple brain scans. A computerised tomographic (CT) scan or a magnetic resonating imaging (MRI) scan of your brain might be done.
Excessive or abnormal growth of the pituitary gland, if seen, will confirm the diagnosis of a pituitary adenoma.
Treatment
Unlike some other benign tumours of the brain, pituitary adenomas mostly cause disturbances that can be fatal. So, you might need the treatment right away. Usually, the treatment of pituitary adenoma consists of medicine, radiation, and surgery, or a combination of these therapies.
- Medicine – sometimes, the use of medication causes the tumour to shrink in size and you might stop having symptoms.
- Radiation – using high-energy X-rays to kill an abnormal tissue (cancer). This therapy is mostly used to shrink the tumour for these two purposes. Firstly, the decrease in size can relieve you of the symptoms caused by the tumour. Secondly, radiation is required to decrease the size of the tumour before performing surgery. This lowers the risk of damaging the surrounding tissue.
Stereotactic radiosurgery is a special form of radiation therapy, in which a high dose of radiation is targeted precisely towards the adenoma from multiple directions. This is used to kill the cancer cells without damaging the neighbouring tissues
- Surgery – the only possible way to remove the tumour. Endoscopic surgery is usually performed which tends to be less invasive. An endoscopic surgery is done by using very small tools along with a camera inserted into the body via a tube, and in this case through your nasal sinuses (air pockets in your nose). This is termed transsphenoidal surgery. In certain cases, transsphenoidal surgery cannot be used requiring an open skull surgery.
Complications
Some of the complications that you might have due to a pituitary adenoma are:
- Vision loss. The pituitary gland is present in close proximity to the optic nerves. These nerves carry the visual scene from your eyes to your brain. Pituitary adenoma can, therefore, compress these nerves causing visual disturbances and even vision loss.
- Permanent hormone deficiency – it usually occurs after the removal pituitary gland with surgery. The gland cannot produce the hormones and you might need hormonal supplements throughout your life.
- Pituitary apoplexy – this occurs when a pituitary adenoma starts bleeding. It is a very rare condition, however, if it does happen you might feel like you have the worst and most severe headache ever. Pituitary apoplexy requires emergency treatment, usually surgery, and corticosteroids.
Prevention
Like most cancerous cases, pituitary adenomas cannot be prevented as such. A healthy lifestyle can have an overall positive effect on your body cells and keep them working properly.
- American Cancer Society. Accessed 04/6/2017.What are Pituitary Tumors?(http://www.cancer.org/cancer/pituitary-tumors/about/what-is-pituitary-tumor.html)
- American Association of Neurological Surgeons. Accessed 4/6/2017.Pituitary Glands and Pituitary Tumors(http://www.aans.org/Patient%20Information/Conditions%20and%20Treatments/The%20Pituitary%20Gland%20and%20Pituitary%20Tumors.aspx)
- National Cancer Institute. Accessed 4/6/2017.General Information about Pituitary Tumors(http://www.cancer.gov/types/pituitary/hp/pituitary-treatment-pdq)
- American Brain Tumour Association. Accessed 4/6/2017.Pituitary Tumours(https://www.abta.org/tumor_types/pituitary-tumors/)
- Pituitary tumours information page. National Institute of Neurological Disorders and Stroke. https://www.ninds.nih.gov/Disorders/All-Disorders/Pituitary-Tumors-Information-Page. Accessed Oct. 27, 2018.
- Snyder PJ. Clinical manifestations and diagnosis of gonadotroph and other clinically nonfunctioning pituitary adenomas. https://www.uptodate.com/contents/search. Accessed Oct. 27, 2018.
- Loeffler JS, et al. Radiation therapy of pituitary adenomas. https://www.uptodate.com/contents/search. Accessed Oct. 27, 2018.
- Bancos I, et al. Impulse control disorders in patients with dopamine agonist-treated prolactinomas and non-functioning pituitary adenomas: A case-control study. Clinical Endocrinology. 2014;80:863.
- Pituitary tumors treatment — for health professionals. National Cancer Institute. http://www.cancer.gov/types/pituitary/hp/pituitary-treatment-pdq#section/all. Accessed Oct. 27, 2018.
- AskMayoExpert. Prolactinoma. Rochester, Minn.: Mayo Foundation for Medical Education and Research; 2018.
- AskMayoExpert. Cushing syndrome. Rochester, Minn.: Mayo Foundation for Medical Education and Research; 2018.
- Snyder PJ. Treatment of gonadotroph and other clinically nonfunctioning adenomas. https://www.uptodate.com/contents/search. Accessed Oct. 27, 2018.
- Winn RH. Pituitary tumors: Functioning and Nonfunctioning. In: Youmans and Winn Neurological Surgery. 7th ed. Philadelphia, Pa.: Elsevier; 2017. https://www.clinicalkey.com. Accessed Oct. 27, 2018.
- Riggin EA. Allscripts EPSi. Mayo Clinic, Rochester, Minn. Nov. 6, 2020.
- Nieman LK. Medical therapy of hypercortisolism (Cushing’s syndrome). https://www.uptodate.com/contents/search. Accessed Nov. 10, 2020.
- Nippoldt TB (expert opinion). Mayo Clinic. Nov. 23, 2020.
The content shared in the Health Literacy Hub website is provided for informational purposes only and it is not intended to replace advice, diagnosis, or treatment offered by qualified medical professionals in your State or Country. Readers are encouraged to confirm the information provided with other sources, and to seek the advice of a qualified medical practitioner with any question they may have regarding their health. The Health Literacy Hub is not liable for any direct or indirect consequence arising from the application of the material provided.