Relationship between Viral Pneumonia & Ground Glass Opacity
Viral pneumonia is often associated with areas of Ground-Glass Opacity (GGO).
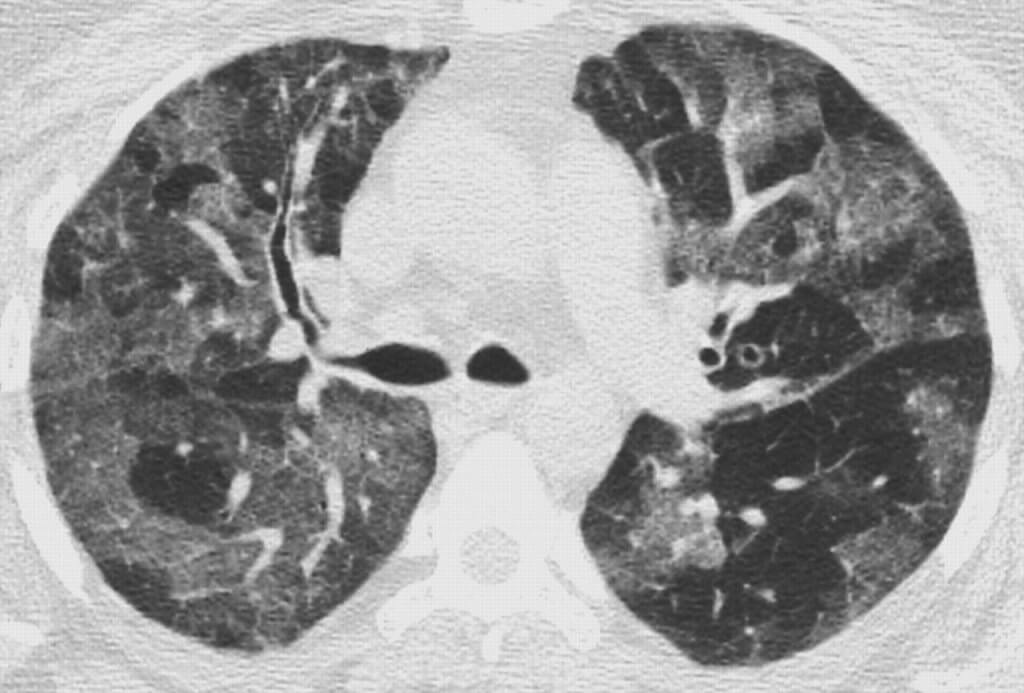
Ground-glass opacity (GGO) is described as an area of increased attenuation of pulmonary structures in the lung parenchyma, usually without obscuring the bronchial-vascular structures. The attenuation, which is identified using conventional imaging procedure, appears on the patient’s medical image as a region more intense compared to the surroundings.
GGO is a visual diagnosis, with the increased attenuation or hazy opacification being captured on chest radiograph using X-ray, or on Computed Tomography (CT) images respectively. The primary cause of GGO is the displacement of air in the lungs by fluid, fibrosis, the collapse of the airway, or a neoplastic process.
Occasionally, radiological images indicate the presence of GGO nodules despite no viral pneumonia. In these cases, a diagnosis of pulmonary edema, interstitial lung disease, or other lung infections may be suspected. In chest radiography and computer tomography, normal lungs appear dark on the images due to lower air density compared to the tissues in the surrounding area.
When a fluid or fibrosis replaces the air, it increases the area density and causes the lung tissue to appear brighter and greyer. Doctors often use ground-glass opacity to describe data or findings in the thoracic scans and perform a differential diagnosis.
Sometimes, ground-glass opacity is used to describe chest radiographs. When it comes to computer tomography, ground-glass opacity is one or multiple areas that have increased density or attenuation without concealing the pulmonary vasculature. That’s why it appears brighter and greyer compared to the normal lungs that appear darker on the image.
On the other hand, ground-glass opacity is one or more areas of the lungs that appear cloudy, hazy, or opaque in chest radiographs. Health professionals use it to describe increased density in both focal and diffuse areas.
Halo sign, mosaic, crazy paving, diffuse, nodular, reversed halo sign and centrilobular mosaic are subtypes of ground-glass opacity.
In this article, we discuss this subject in detail.
Causes of Ground Glass Opacity
There are many causes of ground-glass opacity, such as infections, neoplasm, pulmonary hemorrhage, pulmonary edema, and interstitial lung diseases. Areas of ground-glass attenuations also represent a hallmark for Chronic Obstructive Pulmonary Disease (COPD).
Research studies have shown that CT imaging is effective in finding the clinical features of the patient concerning ground-glass opacities. It can streamline the process of differential diagnosis and accurately find the cause of the problem.
Although ground-glass opacity also appears on the CT images for normal lungs, the term refers to an area of increased attenuation that does not overlay the vascular and bronchial structures. In the presence of certain respiratory diseases, the patient’s lung capacity is reduced due to the presence of fluids or cells in the pleural cavity, or the thickening of either the pleura or the alveolis’ walls (interstitial thickening). In these cases, the air volume is decreased and the density of the tissue on the medical image is increased, thus revealing the characteristic increased attenuation.
A patient who lays flat on the exam table during the imaging procedure has lungs in the posterior position. This can partially collapse their posterior alveoli. Consequently, it causes an increase in tissue density that results in more attenuation. So much so, the chances of the appearance of ground-glass opacity increase on the CT image.
In most cases of bacterial pneumonia and viral pneumonia, a CT imaging procedure enables an accurate diagnosis of the presence of ground-glass opacity. Infections caused by bacteria can cause lobar consolidation. On the other hand, atypical pneumonia usually leads to the formation of ground-glass opacities.
Microbial Causes of Ground-Glass Opacity
Some bacterial infections, such as legionella pneumophilia, chlamydophila pneumoniae, and mycoplasma pneumoniae can cause diffuse sub-type ground-glass opacities in the lungs. Nodular and focal ground-glass opacities are caused by septic emboli and mycobacterium.
Some viruses can also cause this condition in the lungs. The most common viruses responsible for ground-glass opacities are adenovirus, influenza, HMPV, herpes simplex virus, cytomegalovirus, and coronavirus.
Recent research studies have shown that coronaviruses, such as SARS-CoV, MERS-CoV, and SARS-CoV-2 (Covid-19) can also lead to the formation of ground-glass opacity in the lungs. Some studies show that varicella-zoster, measles, and respiratory syncytial viruses are also responsible for nodular, focal, and diffuse opacities.
Fungal infections caused by Pulmonary Cryptococcus, Invasive Aspergillosis, and Candidiasis can lead to the development of ground-glass opacities in the lungs. Studies show that the lungs appear much brighter on the chest CT images due to the presence of opacities caused by fungus.
Types of Ground Glass Opacity
Research highlights that there are 7 sub-types of ground-glass opacities. Typically, the doctor determines the subtype by combining the signs and symptoms of the patient. Computed tomography is one of the best tools to diagnose the presence of ground-glass opacity in different areas of the lung as it helps the health professional simplify the differential diagnosis. Keep in mind that some health conditions of the lung can show a single subtype on the medical image while others can present multiple subtypes of the ground-glass opacity.
The diffuse subtype is characterized by the presence of ground-glass opacities in multiple lobes of both lungs due to the displacement of air with fluid. Other causes include fibrosis and inflammatory debris.
A lung filled with fluid can be caused by cardiogenic pulmonary edema. Diffuse subtype opacity is also caused by alveolar hemorrhage. Most often, doctors diagnose it in various types of health conditions, such as various forms of autoimmune disease, bleeding disorders, and vasculitis.
Moreover, diffuse subtype opacity can also be caused by inflammatory conditions and fibrosis. It is also diagnosed in patients suffering from pneumocystis pneumonia. Studies show that diffuse subtype opacity appears on the scans of patients suffering from AIDS.
Similarly, some forms of pneumonia caused by a viral infection can cause a pattern of diffuse ground-glass opacity in the lungs. One of the adverse effects of pulmonary radiation therapy is known as radiation pneumonitis, which causes pulmonary fibrosis with the formation of diffuse ground-glass opacities observed on the patient’s scan.
Nodular subtype opacity forms in the lungs due to different conditions categorized into benign and malignant disorders. Some benign conditions, such as thoracic endometriosis, pulmonary Cryptococcus, pulmonary contusion, and focal interstitial fibrosis are the leading causes of nodular subtype opacities.
However, studies show that organizing pneumonia, acute eosinophilic pneumonia, and aspergillosis can also lead to the formation of nodular subtype opacities in the lungs. Most often, it is difficult for health professionals to differentiate malignant nodular opacities due to focal interstitial fibrosis. The reason is that this disease creates malignant nodular opacities that are very similar to benign ones.
The malignant cause of nodular ground-glass opacities can be classified as adenocarcinomas and atypical adenomatous hyperplasias. Some research studies have highlighted that 80% of nodular subtype opacities that appear on CT images can represent either pre-malignant or malignant growths.
It is often difficult for radiologists to perform a differential diagnosis between the two based on the radiological images; however, the images produced by the scan machine for nodular opacities can still show some features of pre-malignant nodules that may transform into lung cancer over time.
Pulmonary atypical adenomatous hyperplasia is one of the causes of this subtype opacity. This tumour appears as well-defined round nodular GGO lesions, and depending on the size, biopsy collection and surgical recession of the nodule may be required. In most cases, the size of these lesions is small and less than 6 mm. However, if the size of these structures is larger, a close follow-up is required.
Besides, atypical adenomatous hyperplasia does not have any speculated appearance and solid features on the CT images because it is characterized by malignant growths. On the other hand, when an adenocarcinoma becomes invasive, it leads to retraction of pleura and appears on the image easily. The nodules are usually greater than 15mm, which indicates the presence of invasive lung adenocarcinoma.
A halo sign is a ground-glass opacity shown on the CT image and characterized by an area filled around a nodule or consolidation. Like diffuse opacity, the halo sign is one of the most common types that appeared on the CT images for patients that have pulmonary infections. These are no-cardia infection, tuberculosis, CMV pneumonia, and septic emboli.
Another lung disease known as schistosomiasis is caused by a parasitic infection. It is a disorder that usually appears with the halo sign on the CT scan image. Idiopathic interstitial pneumonia, pulmonary hemorrhage, metastatic disease, and granulomatosis with polyangiitis are non-infectious causes of halo sign subtype ground-glass opacity.
A reversed halo sign is another type of ground-glass opacity, which is characterized by a dense consolidation. Research studies have shown that the consolidation leads to the formation of most of the circle, which is usually 2mm in thickness.
Organizing pneumonia is the leading cause of a reserved halo sign subtype opacity. However, some studies show that the condition does not affect many people. It is also present in lung infarction where the hemorrhage is present in the halo. Other infectious diseases like sarcoidosis, aspergillosis, tuberculosis, and granulomatosis can also cause “reversed halos sign” opacities.
A mosaic ground-glass opacity appears on multiple areas in the lungs. The areas where it is present have both increased and decreased attenuation on the CT image. The obstruction of small airways and occlusion of pulmonary arteries can cause trapping of air.
As a result, the lung develops a mosaic pattern of ground-glass opacities. This subtype opacity is also caused by sarcoidosis, which develops due to granulomas formation in the interstitial areas. Granulomatosis with polyangiitis is another cause of mosaic opacity in the lungs. It causes diffuse areas with an increased attenuation that have a ground-glass appearance.
Crazy paving is another subtype of opacity caused by an interlobular and intralobular widening in the lungs. This ground-glass opacity appears like a road paved with tiles and bricks arranged in irregular patterns. Normally, it is present in one or multiples lobes of the lung.
Crazy paving is caused by a wide range of health conditions, such as pulmonary edema, late-stage adenocarcinoma, and pneumocystis pneumonia. Research shows that pulmonary alveolar proteinosis, sarcoidosis, and diffuse alveolar hemorrhage can also lead to the formation of this subtype ground-glass opacity. Moreover, SARS-CoV-2 or Covid-19 can also cause crazy paving. However, it happens rarely.
Centribular subtype is present in the multiple lobules of the lung. Most often, they occur in secondary lobules of different areas of the lung. Centrilobular appears in the secondary lobules that consist of a small pulmonary artery, bronchiole, and surrounding tissues.
One feature that differentiates Centrilobular subtype ground-glass opacity is no involvement of the interlobular septa. Cholesterol granulomas, aspiration pneumonitis, hypersensitivity pneumonitis, and various types of idiopathic interstitial pneumonias are the primary causes of centrilobular subtype opacity.
Pulmonary cysts and Ground-Glass Opacities
It is an abnormal pattern that commonly appears on the imaging findings for patients with lung conditions. Usually, it is a non-specific finding on the CT scan image. When it comes to differential diagnoses of the pulmonary cyst, it is very limited on the CT scan images. However, it is still characterized by a wide range of health conditions.
A doctor can see the combination of pulmonary cysts and ground-glass opacities in hypersensitivity pneumonitis and desquamative interstitial pneumonia. Cysts rarely occur in these diseases, but if cysts do occur in them, they are fewer in number.
Traumatic pulmonary pseudocysts and hemorrhagic pulmonary metastases can have similar imaging aspects, especially when they are accompanied by pulmonary hemorrhage. In general, the clinical history is enough to diagnose these two health conditions. Lymphocytic interstitial pneumonia is another condition characterized by the combination of pulmonary cysts and ground-glass opacities.
Lymphocytic Interstitial Pneumonia
It can occur in people infected with HIV, Epstein-Barr virus, and with immunodeficiency from other causes. The systemic lupus erythematosus and Sjogren’s syndrome are common systemic diseases diagnosed in immunocompromised individuals.
Chest pain, weight loss, cough, and dyspnea are common clinical manifestations of these two health conditions. In most situations, a CT scan will show a combination of cysts, nodules, consolidation, and ground-glass opacities.
Pneumocystosis
Most patients with HIV that undergo CT scan exams show signs of pneumocystosis. Research shows that patients who use immuno-suppressants and receive bone marrow transplants also show signs of pneumocystosis. Although the symptoms are not clear, some of them are dyspnea, low-grade fever, and dry cough. The condition can lead to respiratory failure and even death.
The combination of medical history, physical exam, increase serum levels of lactate dehydrogenase, and lymphopenia can ease the process of diagnosis. Moreover, the condition is caused by a fungus that can be identified in Bronchoalveolar lavage fluid and sputum.
Furthermore, the finding on the CT scan image shows extensive ground-glass opacities without septal thickening. Sometimes, these opacities also have thickness. Cysts are common and have a predilection of the lobes in the upper lungs.
COVID-19 and Ground-Glass Opacities
Ground-glass opacity is also common in patients suffering from the novel coronavirus or Covid-19. A recently published review study highlighted that Covid-19 patients that underwent radiological imaging procedures showed abnormal chest CT findings. The study showed that 80% of patients had ground-glass opacities and 50% of patients have the combination of consolidation and ground-glass opacities.
Keep in mind that ground-glass opacities with mixed consolidation mostly occur in elderly people. That’s the reason Covid-19 impacts people with pre-existing conditions and those who are above the age of 60. The chest CT scan for Covid-19 shows the bilateral ground-glass opacities at the sides or border areas of the lungs.
During the early stages of Covid-19, the opacities appear on the lower lobes of the lung. Several research studies have confirmed this by analyzing the CT images of the early-stage Covid-19 patients.
Studies show that SARS CoV 2 infection cause a different pattern of opacities in the lungs. Although SARS and MERS along with SARS-CoV-2 belong to the same family of coronaviruses, Covid-19 leads to the formation of a different opacity in the lung. Again, it appears in the lower lobes of the lungs.
With the progression of the disease, ground-glass opacities appear in diffuse subtype that eventually leads to the formation of consolidation. Sometimes, the opacities also appear in the form of the crazy paving pattern with increased septal thickening of the interlobular area.
In most situations, the CT images show that the pulmonary abnormalities occur within two weeks after the Covid-19 symptoms are prominent in the patient. That’s why most patients with Covid-19 show resolution of ground-glass opacities and consolidation on the CT scan images. Acute pulmonary embolism also represents one of the complications for covid patients.
Create stylish call-to-action buttons with Qubely Buttons. Play around with typography, design, border and more. Add animations and personalize it to engage visitors instantly.
Final Words
In conclusion, ground-glass opacities are characterized by a wide range of clinical symptoms and health conditions of the lungs. The most common causes of glass-ground opacities are inflammation, interstitial fibrosis, and hemorrhage. Both benign and malignant conditions can cause them. However, the appearance of opacities on the CT scan images are different for both of them.
Again, it is an abnormal finding on the CT image that has a hazy opacity and does not obscure the pulmonary vessels and bronchial structures. Some ground-glass opacities have no solid components. However, some ground-glass opacities have solid components. Most often, doctors diagnose pulmonary nodules with opacities, which are seen on the high-resolution images produced by the CT scan of the chest.
Computed tomography or CT scan is an advanced medical imaging machine or tool to detect a wide range of abnormalities in hard and soft tissues. It uses x-ray radiations that are passed through the patient’s body and these radiations bounce back to the machine where a computer process the data to produce images. CT is the best tool to diagnose ground-glass opacities in the lungs.
If you have been referred for a medical scan, read this article to find out how to best prepare for it!
The content shared on the Health Literacy Hub website is provided for informational purposes only and it is not intended to replace advice, diagnosis, or treatment offered by qualified medical professionals in your State or Country. Readers are encouraged to confirm the information provided with other sources and to seek the advice of a qualified medical practitioner with any question they may have regarding their health. The Health Literacy Hub is not liable for any direct or indirect consequence arising from the application of the material provided.