3D Anatomy Model
Add another dimension to your learning with fully-interactive educational male and female anatomical models.
Learning about the human anatomy has never been more fun!
Purchase
The cavernous sinus constitutes a component of dural venous sinus within the brain and consist of multiple neurovasculatures. It is located bilaterally to the sella turcica, extending to the petrous part of the temporal bone in the posterior region, and the superior orbital fissure in the anterior part. It is approximately 2 cm long and 1 cm wide. Intercavernous sinuses form the interconnection between right and left cavernous sinuses, present anterior and posterior to the pituitary gland infundibulum.
Let’s start by taking a look at the skull. Explore the model in 3D or click on the AR or VR icons at the bottom right for an immersive exploration.
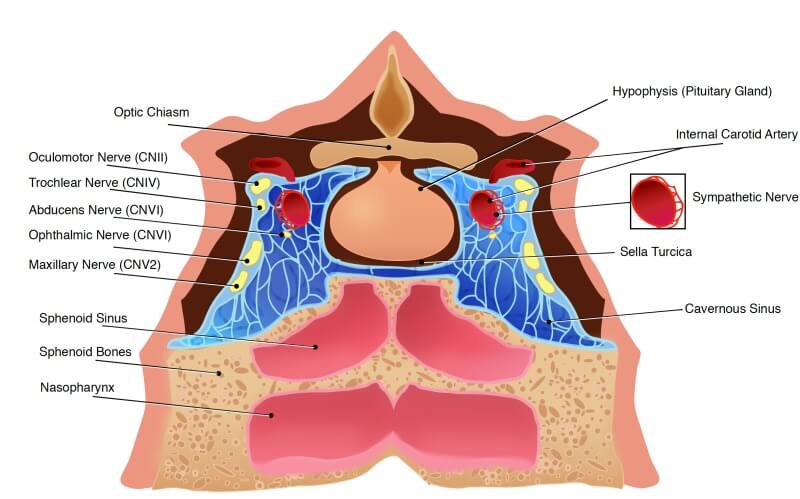
The cavernous sinus acts as a conduit. Before entering the orbit to innervate the eye muscles (both extraocular and intrinsic muscles) the cranial nerves travel through the cavernous sinus once they have left the brainstem. Additionally, drainage of several venous tributaries takes place into the cavernous sinus.
Venous blood from the central retinal, ethmoidal, vorticose, and nasofrontal veins is collected by the superior ophthalmic vein before draining into the cavernous sinus anterior part via the superior orbital fissure. On the other hand, the inferior ophthalmic vein (IOV) collects blood from different structures including the lacrimal sac, eyelids, the vorticose vein, and the orbit’s anterior and medial wall. Furthermore, the IOV divides into two branches after passing toward the lower part of the orbit posteriorly. One of the branches drains into the pterygoid plexus, while the other one joins the cavernous sinus. The origin of the superficial middle cerebral occurs on the lateral portion of the hemisphere. This vein travels through the lateral sulcus, draining the majority of the temporal lobe into the cavernous sinus. Before draining into the cavernous sinus, blood is received by the sphenoparietal sinus from few branches of the middle meningeal vein.
Importantly, another important vein namely efferent hypophyseal veins also drain into the cavernous sinus. Venous blood from all these different veins is collected and then the cavernous sinus drains to the superior and inferior petrosal sinuses. After this it joins the sigmoid sinus, thereby forming the internal jugular vein. The exit of the internal jugular vein from the brain takes place via the jugular foramen, which joins the subclavian vein to form the brachiocephalic vein (right and left).
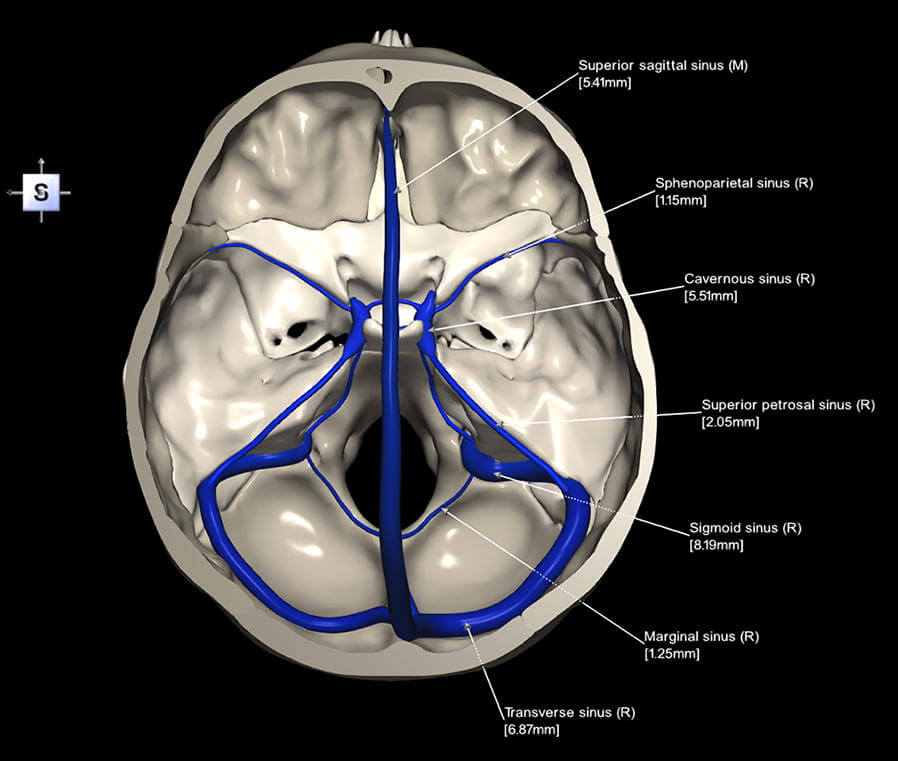
The cavernous sinus is a venous sinus that receives blood from veins including the superior and inferior ophthalmic veins and superficial cortical veins. Typically, it works as a conduit where two important channels drain. This includes the superior and inferior petrosal sinuses draining into the IJV through the sigmoid sinus. In addition, drainage with emissary veins, which pass through the foramina in the skull, takes place into the pterygoid plexus. Anatomically, the cavernous sinus is the only location where an artery (internal carotid artery) passes through a venous structure.
The bifurcation of the common carotid artery occurs in the cervical region giving rise to the internal and external carotid arteries. Superiorly, the internal carotid artery travels and via the carotid canal enters the skull. Following this, the internal carotid artery enters the carotid canal and makes a 90-degree turn, travelling in the horizontal direction in the petrous part of the temporal bone. This is called the petrous part of the internal carotid artery which makes its entrance into the cavernous sinus through the foramen lacerum. The internal carotid artery that enters the cavernous sinus is also called the cavernous part. This cavernous part turns horizontally and anteriorly till it reaches the sinus up to the anterior limit. From there onwards, it curves vertically and exits the sinus from the superior aspect. It becomes the internal carotid artery’s cerebral part.
The different cranial nerves of the cavernous sinus are the oculomotor nerve (CN III), trochlear nerve (CN IV), ophthalmic nerve (V1), maxillary nerve (V2), and abducens nerve (CN VI). Around the internal carotid artery, there is the sympathetic plexus. The oculomotor nerve makes an exit ventrally through the interpeduncular fossa and pierces the dura. It enters the cavernous sinus and runs on the lateral wall and roof. The origin of the trochlear nerve is from the trochlear nerve nucleus. Inferiorly, it emerges from the inferior colliculus which is present in the posterior part of the midbrain.
The ophthalmic nerve and the maxillary nerve are branches of the trigeminal nerve (CN V). The trigeminal nerve exits the brainstem via the ventrolateral pons and passes through the Meckel’s cave where the trigeminal ganglion is present. The ophthalmic nerve passes through the inferior portion of the cavernous sinus and exits the cavernous sinus. It enters the orbit through the superior orbital fissure. The abducens nerve pierces the dura after exiting the brainstem ventrally from the pontomedullary junction. It travels a long intracranial course and enters the cavernous sinus, surrounded by venous blood.
The superior cervical ganglion gives origin to the sympathetic plexus. The sympathetic plexus is present around the internal carotid artery, travels along with it and passes through the carotid canal to enter the skull making an entrance into the cavernous sinus through the jugular foramen.
Cavernous sinus syndrome is a life-threatening emergency with a wide spectrum of clinical symptoms depending on the target structure that is affected. Any severe lesion that damages the cavernous sinus entirely will result in complete ophthalmoplegia as a result of injury to cranial nerves III, IV and VI. Other clinical symptoms include fixation and dilation of pupils caused due to superficial parasympathetic fibres compression of the CN III.
Cavernous sinus syndrome may also cause Horner’s syndrome. This syndrome occurs due to the damage of the sympathetic plexus located around the internal carotid artery. Damage to cranial nerves V1 and V2 may lead to loss of sensory sensation around several structures such as maxilla, nasal cavity, face, scalp, sinuses, and palate.
The main etiology of cavernous sinus syndrome includes granulomatous diseases, metastatic tumour, meningioma, pituitary tumour, an extension of the nasopharyngeal tumours, cavernous sinus thrombosis and aneurysms of the cavernous part of the internal carotid artery.
Rupture of the cavernous aneurysm may lead to carotid-cavernous fistula, resulting in pulsating exophthalmos.
Blood from the facial vein may also drain to the cavernous sinus in certain cases promoting a pathway for infection. This may cause the infection to spread from the face to the cavernous sinus, and from there to the brain.
1.Ipsalali HO, Ciftci AC, Kilic D, Sendemir G, Seyhan S, Kaya I, Ortug G. Variations of the 6th cranial nerve (nervus abducens) in the petroclival region: A microsurgical study. Morphologie. 2019 Jun;103(341 Pt 2):103-109.
2. Ngnitewe Massa R, Minutello K, Mesfin FB. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Jul 27, 2020. Neuroanatomy, Cavernous Sinus.
3.Graffeo CS, Perry A, Copeland WR, Raghunathan A, Link MJ. Histology of the distal dural ring. Clin Anat. 2017 Sep;30(6):742-746.
4. Patel CR, Fernandez-Miranda JC, Wang WH, Wang EW. Skull Base Anatomy. Otolaryngol Clin North Am. 2016 Feb;49(1):9-20.
5. Klinger DR, Flores BC, Lewis JJ, Barnett SL. The treatment of cavernous sinus meningiomas: evolution of a modern approach. Neurosurg Focus. 2013 Dec;35(6):E8.
6. Park HS, Chung MS, Shin DS, Jung YW, Park JS. Whole courses of the oculomotor, trochlear, and abducens nerves, identified in sectioned images and surface models. Anat Rec (Hoboken). 2015 Feb;298(2):436-43.
7.Duong DK, Leo MM, Mitchell EL. Neuro-ophthalmology. Emerg Med Clin North Am. 2008 Feb;26(1):137-80, vii.
The content shared in the Health Literacy Hub website is provided for informational purposes only and it is not intended to replace advice, diagnosis, or treatment offered by qualified medical professionals in your State or Country. Readers are encouraged to confirm the information provided with other sources, and to seek the advice of a qualified medical practitioner with any question they may have regarding their health. The Health Literacy Hub is not liable for any direct or indirect consequence arising from the application of the material provided.